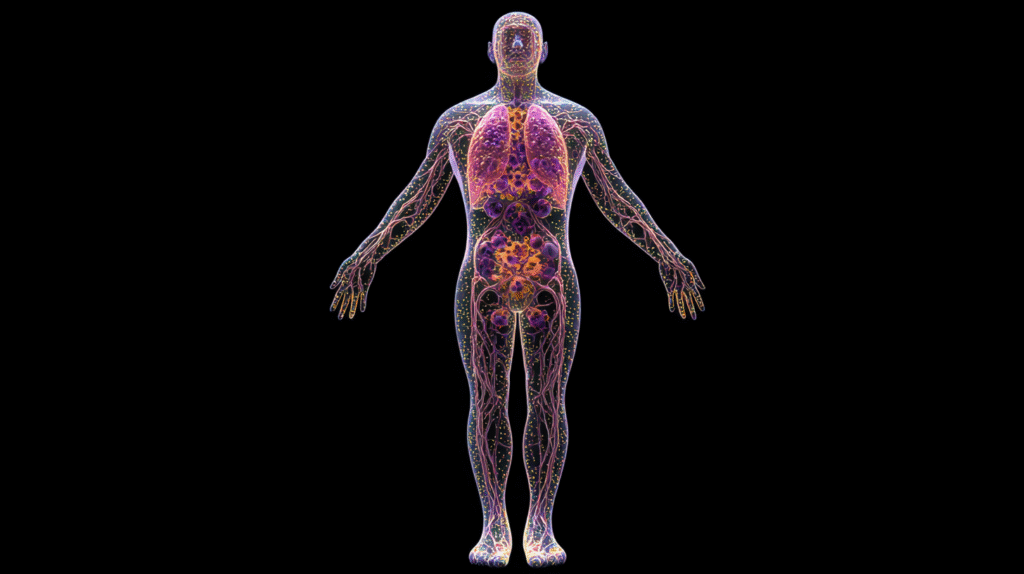
Autoimmune diseases can feel like a mystery, leaving you with questions about what’s happening inside your own body. These conditions occur when your immune system—which is designed to protect you from harmful invaders like bacteria and viruses—turns rogue and starts attacking your healthy tissues instead. The result? A wide variety of symptoms that vary depending on the specific autoimmune disease.
This post takes a closer look at some of the most common autoimmune diseases, including lupus, rheumatoid arthritis (RA), and psoriasis, among others. We’ll break down their symptoms, causes, and treatment options while highlighting what makes each condition unique. Whether you’re looking for information to better understand your own diagnosis or to support someone you care about, this guide has you covered.
What Are Autoimmune Diseases?
Before we jump into specific conditions, let’s first define autoimmune diseases. Simply put, an autoimmune disease occurs when your immune system mistakenly attacks your body’s healthy cells. Think of your immune system like a security team meant to guard against invaders—but sometimes, it identifies the “good guys” as threats, leading to inflammation, pain, and damage.
There are more than 80 known autoimmune diseases. Some target specific organs (like Type 1 diabetes with the pancreas), while others can affect multiple systems throughout the body. Below is a list of autoimmune diseases we’ll focus on today, with a deeper look into the top three most common ones.
List of Common Autoimmune Diseases
- Lupus (Systemic Lupus Erythematosus)
- Rheumatoid Arthritis (RA)
- Psoriasis and Psoriatic Arthritis
- Multiple Sclerosis (MS)
- Hashimoto’s Thyroiditis
- Graves’ Disease
- Type 1 Diabetes
- Inflammatory Bowel Diseases (Crohn’s and Ulcerative Colitis)
Each of these diseases has unique characteristics, but they also share a common thread of immune system dysfunction.
Lupus (Systemic Lupus Erythematosus): The “Great Imitator”
What Is Lupus?
Lupus is a chronic autoimmune condition that can affect multiple parts of the body, including the skin, joints, kidneys, heart, and brain. Because its symptoms overlap with so many other diseases, lupus is often called the “great imitator.”
Symptoms of Lupus:
- Persistent fatigue
- Joint pain and swelling
- Butterfly-shaped rash on the cheeks and nose
- Sensitivity to sunlight
- Hair loss
- Kidney problems
- Chest pain
Causes:
The exact cause of lupus isn’t fully understood, but researchers believe it’s a combination of genetics, hormonal changes, and environmental factors like infections or exposure to sunlight. Lupus is also far more common in women than men, with estrogen possibly playing a role.
Lupus vs Rheumatoid Arthritis:
Both lupus and RA can cause joint pain and inflammation, but they differ in how they impact the body. RA specifically targets joints, leading to destruction and deformity, whereas lupus is more systemic and may involve vital organs like the kidneys and heart.
Treatment for Lupus:
- Anti-inflammatory medications and pain relievers
- Immunosuppressants to calm the immune system
- Corticosteroids for severe inflammation
- Lifestyle changes, including sun protection and stress management
Rheumatoid Arthritis (RA): When Your Joints Are Under Attack
What Is Rheumatoid Arthritis?
RA is a chronic autoimmune disease that primarily affects the joints. It happens when the immune system attacks the synovium, the lining of the joints, leading to pain, stiffness, swelling, and eventual joint destruction if left untreated.
Symptoms of RA:
- Morning stiffness that lasts longer than an hour
- Swollen, red, or tender joints (most commonly in the hands, wrists, and knees)
- Fatigue and low-grade fever
- Bumps or nodules under the skin (rheumatoid nodules)
Causes:
Like lupus, RA’s exact cause isn’t fully known. However, a combination of genetic predisposition, environmental triggers (like smoking), and possibly hormonal influences may set the stage for this disease.
Treatment for RA:
- DMARDs (disease-modifying anti-rheumatic drugs): Medications like methotrexate slow disease progression.
- Biologics: Target specific parts of the immune system to reduce inflammation.
- Lifestyle modifications, including physical therapy, exercise, and anti-inflammatory diets.
Lupus vs. RA:
While both share joint pain as a symptom, RA almost exclusively targets the joints, often leading to deformities, whereas lupus has a broader systemic impact.
What Is Psoriasis? An Overview of This Autoimmune Skin Disease
What Is Psoriasis Autoimmune?
Psoriasis is an autoimmune condition that primarily affects the skin but can also lead to psoriatic arthritis when it involves the joints. The disease accelerates the life cycle of skin cells, causing them to build up rapidly on the surface. The result? Flaky, silvery patches of skin and persistent itching.
Symptoms of Psoriasis:
- Raised, red patches (plaques) covered with white or silvery scales
- Dry, cracked skin that may bleed
- Itching, burning, or pain around affected areas
- Thickened or ridged nails
What Is Psoriatic Arthritis?
Some people with psoriasis also develop psoriatic arthritis (PsA), which causes joint pain, swelling, and stiffness similar to RA. PsA tends to affect the smaller joints in the hands and feet but can also involve the spine.
Causes:
Psoriasis runs in families, but environmental triggers such as stress, infections, or certain medications often bring on flare-ups.
Treatment for Psoriasis and Psoriatic Arthritis:
- Topical treatments like corticosteroids or salicylic acid to reduce itching and scaling
- Phototherapy (light therapy) to slow cell turnover
- Biologic drugs for severe cases
- Anti-inflammatory diets may also help reduce flare-ups.
Lupus, RA, and Psoriasis Comparison:
While lupus and RA involve systemic inflammation that often targets the joints, psoriasis is more apparent on the skin. However, psoriatic arthritis demonstrates how the condition can overlap with joint-related autoimmune diseases.
Other Notable Autoimmune Diseases
While lupus, RA, and psoriasis are among the most well-known autoimmune diseases, here are a few other important ones to note.
1. Multiple Sclerosis (MS)
Symptoms: Numbness, muscle weakness, and visual disturbances caused by immune cells attacking the protective sheath around nerves in the brain and spinal cord (myelin).
Treatment: Disease-modifying therapies slow progression, alongside physical therapy and symptom management.
2. Hashimoto’s Thyroiditis and Graves’ Disease
Hashimoto’s: Causes an underactive thyroid (hypothyroidism) with symptoms like fatigue, weight gain, and sensitivity to cold.
Graves’: Triggers an overactive thyroid (hyperthyroidism), leading to symptoms like rapid heartbeat, weight loss, and anxiety.
Treatment: Hormone replacement for Hashimoto’s; medications or radioactive iodine for Graves’.
3. Type 1 Diabetes
Symptoms: High blood sugar, frequent urination, extreme thirst, and unplanned weight loss as the immune system destroys insulin-producing cells in the pancreas.
Treatment: Insulin therapy and a well-balanced diet.
4. Inflammatory Bowel Diseases (IBDs)
Both Crohn’s Disease and Ulcerative Colitis cause chronic inflammation in the digestive tract, often leading to abdominal pain, diarrhea, and nutritional deficiencies.
Lesser-Known Autoimmune Diseases
While conditions like lupus, rheumatoid arthritis, and psoriasis grab most of the spotlight, there are many lesser-known autoimmune diseases that also deserve attention. Here are a few you may not have heard about but are equally important to understand.
1. Sjögren’s Syndrome
This autoimmune disease targets the glands that produce moisture in the body, leaving you with dry eyes, dry mouth, and even trouble swallowing. It can also lead to joint pain and fatigue. Many people with Sjögren’s also have another autoimmune disease like RA or lupus.
Key management strategies:
- Use artificial tears or prescription eye drops for dryness.
- Stay hydrated and consider saliva-stimulating medications for dry mouth.
- Work with your healthcare provider to manage joint pain and fatigue.
2. Dermatomyositis
This condition causes inflammation in muscles and skin, leading to muscle weakness and a noticeable rash. The rash often appears purple or red and can show up on the face, chest, or hands.
Key management strategies:
- Use immunosuppressants and corticosteroids to control inflammation.
- Engage in physical therapy to improve muscle strength and mobility.
3. Autoimmune Hepatitis
This is a rare condition where the immune system attacks the liver, potentially causing scarring and liver damage if left untreated.
Key management strategies:
- Immunosuppressant medications to slow the attack on the liver.
- Regular liver function monitoring and a diet supportive of overall liver health.
4. Vasculitis
Vasculitis involves inflammation of blood vessels, which can affect any organ in the body. Symptoms vary depending on which blood vessels are involved, but common signs include fatigue, fever, and localized pain.
Key management strategies:
- Corticosteroids and immunosuppressant drugs to reduce inflammation.
- Regular medical care to monitor for complications like organ damage.
These lesser-known autoimmune diseases highlight the complexity of immune system dysfunction and the need for personalized treatment approaches.
The Role of Genetics in Autoimmune Conditions
One question that commonly arises is, “Do autoimmune diseases run in families?” The answer lies in genetics—but it’s not the whole story.
Genetic Predisposition to Autoimmune Diseases
Having a relative with an autoimmune disease increases your risk of developing one yourself, but the specific condition may vary. For example, your mom might have rheumatoid arthritis while you develop lupus. Scientists believe this is because certain genetic markers, like HLA (human leukocyte antigen), make people more susceptible to immune system malfunctions.
The Environment’s Role in Activating Genes
Genetics lays the groundwork for susceptibility, but environmental factors often “pull the trigger.” Common triggers include:
- Stress
- Viral or bacterial infections
- Toxins or pollutants
- Hormonal changes (such as pregnancy or menopause)
Researchers call this interaction the “genetic-environmental interplay.” Essentially, you might inherit the potential for an autoimmune disease, but external factors determine if and when it develops.
Family Genetic Testing
If multiple family members have autoimmune diseases, genetic testing may help you assess your own risk. While this doesn’t guarantee you’ll develop a condition, it could encourage earlier monitoring or preventive measures.
How Lifestyle Changes Can Help Manage Symptoms
While modern medicine offers powerful treatments for autoimmune diseases, your day-to-day choices play an equally important role in managing symptoms and preventing flare-ups.
1. Focus on an Anti-Inflammatory Diet
Certain foods help fight inflammation and support your immune system, while others can wreak havoc.
- Foods to add:
- Colorful fruits and vegetables (blueberries, spinach, broccoli)
- Healthy fats like olive oil, avocado, and nuts
- Omega-3-rich fish like salmon and sardines
- Whole grains like quinoa and oats
- Foods to avoid:
- Processed snacks and sugary drinks
- Red meat and fried foods
- Artificial trans fats found in some baked goods
2. Stay Physically Active
Exercise might feel intimidating if you’re battling fatigue or joint pain, but even gentle movements can make a big difference. Physical activity boosts circulation, improves mood, and reduces inflammation over time.
- Consider low-impact exercises like swimming, yoga, or walking.
- Don’t overdo it; listen to your body and rest if needed.
3. Reduce Stress
Chronic stress is a known trigger for autoimmune flares. Managing stress levels keeps both your mind and body in better balance.
- Practice mindfulness through meditation, journaling, or yoga.
- Make time for hobbies or activities that bring you joy.
- Engage in deep-breathing exercises to stay calm during stressful moments.
4. Prioritise Restful Sleep
Fatigue is a hallmark symptom of most autoimmune diseases, which makes quality sleep an absolute must. Build healthy sleep habits, like maintaining a consistent bedtime and creating a soothing pre-sleep routine free of screens or bright lights.
5. Work Closely With Your Healthcare Team
Lifestyle changes are a powerful tool, but they work best when paired with guidance from your medical provider. Share your goals and ask how you can integrate these changes into your current treatment plan.
Taking Control of Autoimmune Diseases
Autoimmune diseases can feel overwhelming, but with the right information and support, managing these conditions becomes much more achievable. Here are some universal tips for living well with autoimmune diseases:
- Educate yourself about your specific condition and triggers.
- Partner closely with your healthcare provider to find treatments that work for you.
- Incorporate anti-inflammatory foods into your diet and stay physically active (but don’t overdo it).
- Practice self-care to help manage stress and prevent flare-ups.
Whether it’s lupus, RA, psoriasis, or any other autoimmune disease, remember you’re never alone in your health journey. There’s a wealth of resources, communities, and treatments available to help you regain control of your life. You’ve got this!